HIPAA
HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT
HIPAA (Health Insurance Portability and Accountability Act) certification is the process of demonstrating compliance with the HIPAA Security and Privacy Rules. Although the U.S. Department of Health and Human Services (HHS) does not endorse an official certification program, organizations can pursue third-party assessments and certifications to validate their adherence to HIPAA requirements.
It involves evaluating an organization’s administrative, physical, and technical safeguards implemented to protect individuals’ healthcare information, known as protected health information (PHI). It includes assessing policies, procedures, technical controls, employee training, and risk management practices to ensure they align with HIPAA regulations.
By obtaining the certification, healthcare organizations can showcase their commitment to protecting patient privacy and security. It can enhance their reputation, foster trust with patients and business partners, and mitigate the risk of costly penalties for non-compliance. The HIPAA certification, although not an official designation, externally validates the organization’s compliance efforts and showcases a proactive approach to safeguarding Protected Health Information (PHI).

HIPAA Compliance Audit Services by CertPro
At CertPro, we have a profound understanding of the importance of protecting personal data and the invaluable role that HIPAA compliance plays in this area. We provide comprehensive support to organizations committed to maintaining data security by pursuing HIPAA compliance. Our team of experienced professionals will assist you throughout the certification process, ensuring that your data protection practices fully adhere to the latest HIPAA standards. Together, we will collaboratively develop and implement a tailored data protection framework that meets your specific needs and industry-related obligations.
Why choose CertPro for HIPAA certification and auditing?
Securing HIPAA compliance is a critical priority for organizations entrusted with personal data. At CertPro, our certification services are designed to simplify the process, guaranteeing that your organization fulfills the rigorous requirements of HIPAA. With our trusted expertise and extensive experience in HIPAA certification and auditing, CertPro stands as a reliable choice. Our exceptional track record and profound understanding of data protection regulations provide compelling reasons to select us as your preferred partner for all your HIPAA certification needs. Trust CertPro to guide you towards a comprehensive and successful HIPAA compliance journey.
| Factors | CertPro Advantage |
|---|---|
| Time to Certification | 4x faster than traditional approaches |
| Price | Competitive rates with flexible options |
| Process | Streamlined and efficient methodology |
| Expertise | 10+ years of industry experience |
CertPro’s Cost-Effective Approach to HIPAA Certification
When it comes to evaluating the costs associated with HIPAA certification, it is crucial to consider various factors that can contribute to the overall expenses. At CertPro, we recognize the importance of adopting a cost-effective approach and strive to provide a customized pricing structure that aligns with the specific requirements of your organization. Here is a breakdown of our approach to HIPAA certification pricing, ensuring transparency and tailored solutions:
| No. of employees | Timeline | Cost (approx.) |
| 1 – 25 | 4 weeks | 2500 USD |
| 25-100 | 6 weeks | 3500 USD |
| 100-250 | 6-8 weeks | 5000 USD |
| 250 plus | 8 weeks | Custom plans |
HIPAA: A Comprehensive Overview
HIPAA certification pertains to the compliance standards established by the Health Insurance Portability and Accountability Act (HIPAA) in 1996. HIPAA certification ensures that organizations handling protected health information (PHI) meet the security and privacy requirements outlined in the act. HIPAA certification entails conducting a comprehensive evaluation of an organization’s policies, procedures, and technical measures aimed at safeguarding patient data against unauthorized access, use, or disclosure. HIPAA certification confirms that an organization has implemented suitable administrative, physical, and technical safeguards to protect PHI, trained its employees on HIPAA regulations, conducted regular risk assessments, and established procedures for incident response and breach notification. Obtaining HIPAA certification indicates an organization’s dedication to maintaining the security and privacy of patient health information.
- The Privacy Rule sets forth standards for safeguarding protected health information (PHI), which encompasses individually identifiable health information. It sets limits on the use and disclosure of PHI, requiring individuals’ consent for certain purposes and granting them rights over their health information.
- The Security Rule, on the other hand, outlines safeguards for electronic PHI (ePHI) to ensure its confidentiality, integrity, and availability. It requires covered entities to implement administrative, physical, and technical safeguards to protect ePHI from unauthorized access or disclosure.
The primary goal of HIPAA (Health Insurance Portability and Accountability Act) is to safeguard the privacy and security of individuals’ protected health information (PHI). It ensures that sensitive health information is protected while allowing for the necessary flow of information for effective healthcare delivery and operations.
HIPAA sets forth standards for the electronic exchange, privacy, and security of health information. HIPAA aims to strike a balance between facilitating the secure and efficient exchange of health data for treatment, payment, and healthcare operations while safeguarding individuals’ privacy rights.
The overarching goal of HIPAA is to establish a comprehensive framework that protects the confidentiality, integrity, and availability of PHI while empowering individuals with greater control over their health information. This is achieved through the implementation of administrative, physical, and technical safeguards by covered entities, such as healthcare providers, health plans, and healthcare clearinghouses.
THE STEPS INVOLVED IN HIPAA CERTIFICATION
Organizations can take the following steps to achieve HIPAA compliance and become certified:
1. Create Privacy and Security Policies for the Organization: Develop comprehensive privacy and security policies that align with the requirements of the HIPAA Privacy Rule and Security Rule. These policies should outline how your organization handles protected health information (PHI) and ensure compliance with HIPAA regulations.
2. Appoint a HIPAA Privacy Officer and Security Officer: Designate individuals within your organization to assume the roles of HIPAA Privacy Officer and Security Officer. These officers will be responsible for overseeing and implementing the organization’s privacy and security policies, ensuring compliance, and handling any related inquiries or incidents.
3. Implement Security Safeguards: Put in place appropriate security safeguards to protect PHI. It includes technical measures such as access controls, encryption, and secure storage of electronic PHI (ePHI), as well as physical safeguards like restricted access to PHI storage areas and secure disposal of physical PHI.
4. Regularly Conduct Risk Assessments and Self-Audits: Perform regular risk assessments to identify potential vulnerabilities and risks to the integrity, confidentiality, and availability of the PHI. Additionally, conduct self-audits to assess your organization’s compliance with HIPAA requirements. These assessments help identify areas for improvement and allow you to take corrective action.
5. Maintain Business Associate Agreements: If your organization shares PHI with business associates, establish written agreements with them. These agreements, known as Business Associate Agreements (BAAs), outline the responsibilities of business associates in safeguarding PHI and complying with HIPAA regulations. Maintain a record of these agreements to demonstrate your organization’s commitment to protecting PHI.
6. Establish a Breach Notification Protocol: Develop a breach notification protocol that outlines the steps to be taken in the event of a data breach or security incident involving PHI. It includes assessing the breach, mitigating the risks, informing the affected parties, and reporting the breach to the appropriate authorities in accordance with HIPAA regulations.
7. Document Everything: Maintain thorough documentation of your organization’s HIPAA compliance efforts. It includes policies and procedures, risk assessments, self-audit reports, training records, breach notification documentation, business associate agreements, and other relevant documentation. Proper documentation demonstrates your organization’s commitment to compliance and helps during audits or investigations.
Finally, achieving and maintaining HIPAA compliance is an ongoing process. It requires continuous vigilance, regular updates to policies and procedures, and staying informed about changes in regulations and best practices.

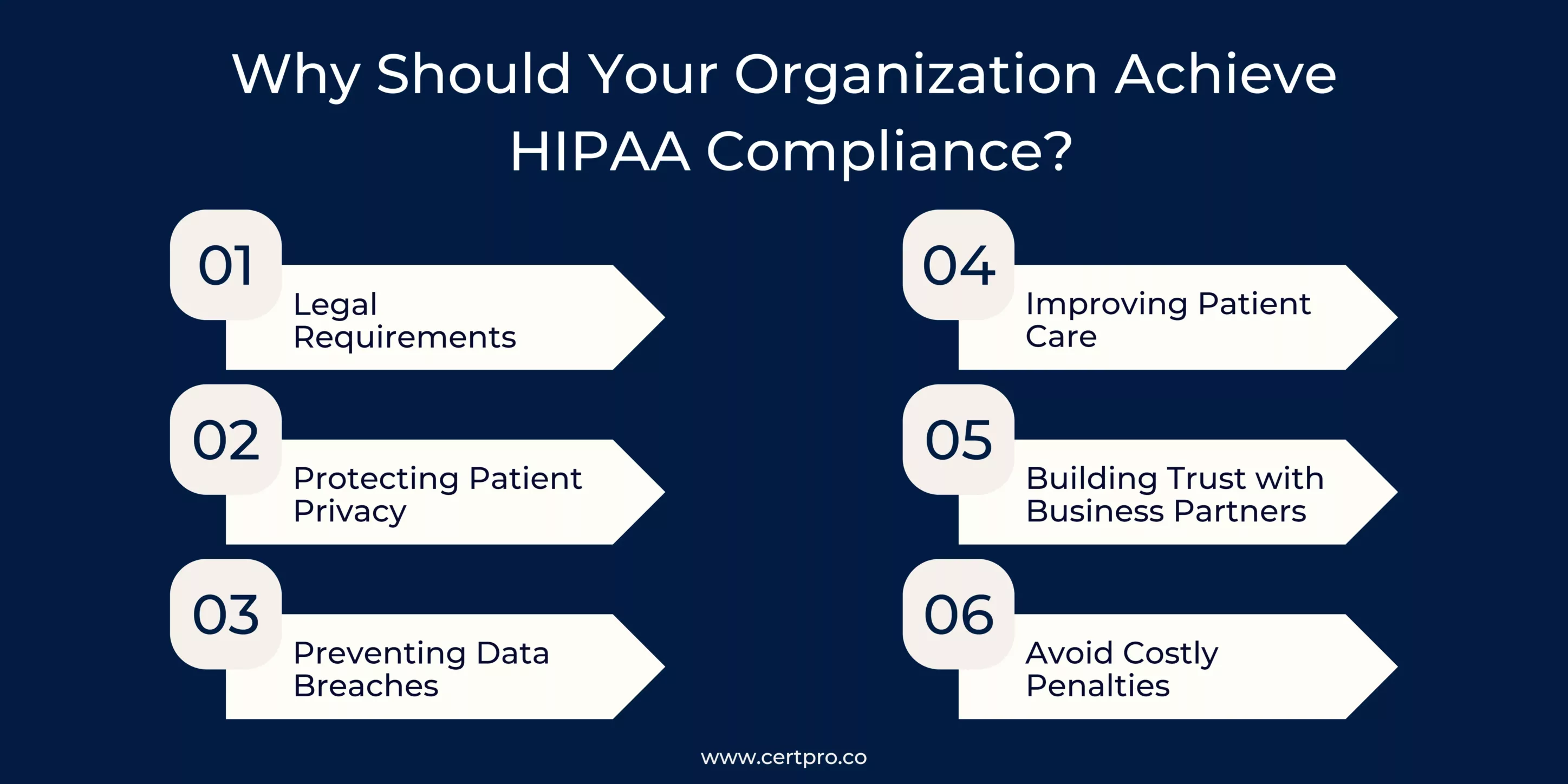
Why should your organization achieve HIPAA compliance?
HIPAA compliance means that the organization is following the standards outlined in the Health Insurance Portability and Accountability Act (HIPAA) for safeguarding protected health information (PHI). Organizations must also provide training to employees on handling PHI and have policies and procedures in place to address security incidents. HIPAA compliance is mandatory for healthcare entities that hold PHI and is crucial for maintaining patient trust and avoiding legal consequences. Becoming HIPAA-compliant is important for several reasons.
- Legal Requirements: HIPAA is a federal law that mandates the protection of patient health information. Compliance ensures organizations meet legal obligations, avoiding penalties and legal consequences.
- Protecting Patient Privacy: HIPAA compliance safeguards patient privacy by implementing strict controls on the storage, access, and sharing of protected health information (PHI). This helps maintain confidentiality and builds trust with patients.
- Preventing Data Breaches: HIPAA compliance enforces robust security measures, such as encryption and access controls, to prevent unauthorized access and data breaches. This protects patients from potential identity theft and fraud.
- Improving Patient Care: Compliance can lead to improved patient care through secure electronic health records (EHRs) and streamlined workflows. Access to accurate and complete patient information enhances care coordination and enables better-informed treatment decisions.
- Building Trust with Business Partners: Compliance demonstrates an organization’s commitment to protecting patient data, making them a trusted partner for collaborations with other healthcare entities. This can facilitate smoother information sharing and partnerships.
- Avoid Costly Penalties: Non-compliance with HIPAA can result in significant financial penalties, ranging from fines to legal consequences. Achieving HIPAA compliance helps you mitigate the risk of violations and associated financial burdens.
What are the HIPAA certification requirements?
1. Privacy Rule: The Privacy Rule establishes standards for protecting individuals’ PHI and their rights to access and control their health information. It requires organizations to implement policies and procedures to safeguard PHI, obtain patient consent for certain uses and disclosures, provide individuals with notice of privacy practices, and ensure the confidentiality of PHI during its transmission and storage.
2. Security Rule: The Security Rule sets standards for safeguarding electronic PHI (ePHI) by implementing appropriate administrative, physical, and technical safeguards. It requires organizations to conduct risk assessments, develop security policies and procedures, provide workforce training, manage access to ePHI, and implement measures to protect against unauthorized access, use, or disclosure.
3. Breach Notification Rule: The Breach Notification Rule outlines the requirements for notifying affected individuals, the Secretary of the Department of Health and Human Services (HHS), and, in certain cases, the media, in the event of a breach of unsecured PHI. Organizations must have policies and procedures in place to promptly identify and respond to breaches and mitigate harm to individuals.
4. Business Associate Agreements: HIPAA requires covered entities (such as healthcare providers and health plans) to enter into written agreements, known as Business Associate Agreements (BAAs), with their business associates. BAAs ensure that business associates, such as vendors and contractors, also comply with HIPAA regulations and appropriately safeguard PHI.
5. Documentation and Recordkeeping: Organizations must maintain documentation and records that demonstrate their compliance efforts, including policies and procedures, risk assessments, training records, incident response plans, and other relevant documentation. These records should be retained for a specified period of time as required by HIPAA.
6. Enforcement: HIPAA provides for enforcement mechanisms to ensure compliance and address violations. The Office for Civil Rights (OCR) within HHS is responsible for enforcing HIPAA rules and may conduct audits, investigations, and impose penalties for non-compliance.
It’s important to note that while there is no formal HIPAA certification, organizations can engage in voluntary audits and assessments conducted by third-party organizations to evaluate their compliance with HIPAA requirements. These assessments can help organizations identify any gaps or areas for improvement and demonstrate their commitment to protecting patient privacy and security.
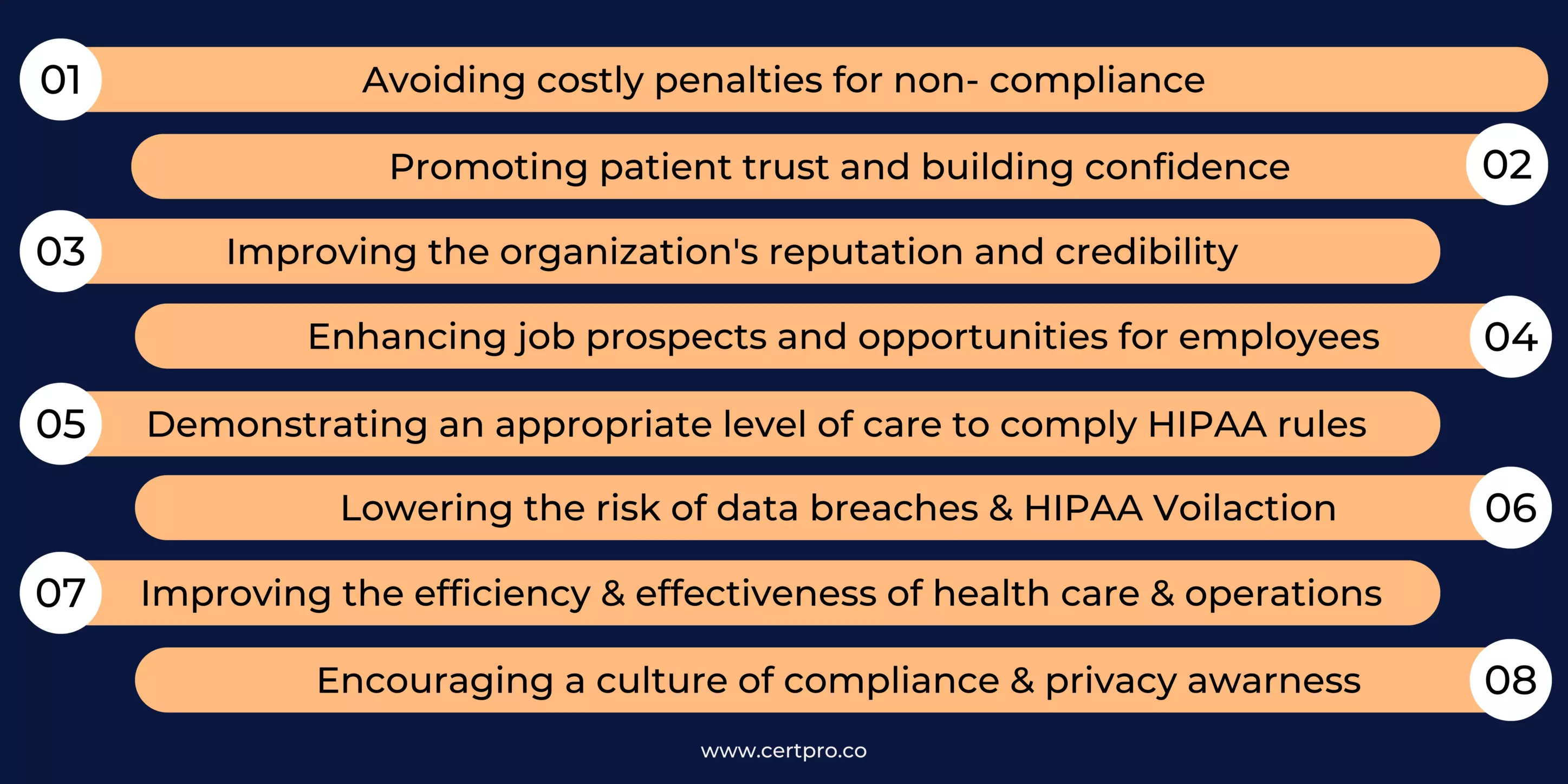
THE BENEFITS OF HIPAA CERTIFICATION
HIPAA certification can provide numerous benefits for healthcare organizations, including increased patient trust, protection against costly penalties for non-compliance, and a competitive advantage in the industry. It also helps to ensure the security and privacy of individuals’ healthcare information, known as Protected Health Information (PHI). HIPAA certification offers the following benefits:
ELIGIBILITY FOR HIPAA CERTIFICATION
HIPAA compliance is not something that individuals or organizations actively seek to obtain or become eligible for. Instead, HIPAA compliance is required for certain entities within the healthcare industry, namely covered entities and their business associates.
- Covered entities include healthcare providers, health plans, and healthcare clearinghouses that electronically transmit health information in connection with specific transactions. Examples of covered entities include hospitals, doctors, dentists, health insurers, and pharmacies.
- Business associates are individuals or organizations that perform certain functions or activities on behalf of covered entities that use or disclose protected health information (PHI). Business associates can include IT service providers, billing companies, medical transcription services, cloud storage providers, and consultants.
Therefore, an entity’s eligibility for HIPAA compliance is determined based on its role and involvement in the healthcare industry. To safeguard patient privacy and ensure the security of health information, an entity must actively comply with HIPAA requirements if it meets the definition of a covered entity or business associate as stated in HIPAA regulations.
COST OF HIPAA CERTIFICATION
The cost of HIPAA certification can vary widely depending on various factors, such as the size of the organization, the complexity of its operations, and the level of assistance sought from external consultants or auditors. Generally, the cost includes expenses related to conducting a risk assessment, developing and implementing policies and procedures, employee training, security measures, and any necessary technology upgrades. Additionally, there may be ongoing costs associated with monitoring, auditing, and maintaining compliance. It’s important to note that the government or a specific certification body does not issue an official HIPAA certification. Therefore, the cost primarily relates to the resources allocated by organizations to achieve and maintain HIPAA compliance.
While there is no HIPAA certification-free option, achieving HIPAA compliance does come with costs. The expenses associated with HIPAA compliance can vary depending on the size and complexity of the organization.
VALIDITY PERIOD OF HIPAA CERTIFICATION
HIPAA compliance is an ongoing commitment rather than a certification with an expiration date. Once an organization achieves HIPAA compliance, it does not have a specific validity period. Compliance requires continuous adherence to HIPAA regulations, including the Privacy Rule, Security Rule, and other relevant provisions. Organizations must consistently assess and update their policies, procedures, security measures, and employee training to address evolving risks and changes in the healthcare landscape. Regular monitoring, audits, and risk assessments are necessary to ensure ongoing compliance. While there is no set time frame for HIPAA validity, organizations should maintain compliance as long as they handle protected health information (PHI) and remain subject to HIPAA regulations.
Supporting Your Business in Achieving HIPAA Certification
CertPro provides auditing, consulting, and certification services to assist businesses in achieving HIPAA certification. Their experienced team of auditors and consultants delivers projects using industry best practices to meet clients requirements and ensure that the latest technological advancements are incorporated. They offer one-stop solutions for all compliance needs, from initial assessments to policy development, employee training, and risk management. CertPro focuses on providing maximum value for clients throughout their compliance journey, ensuring that they achieve HIPAA certification efficiently and effectively. They work closely with clients to ensure that they understand the process and requirements of HIPAA compliance, providing tailored solutions to meet their unique needs. By engaging CertPro, organizations can be confident that they are on the right track to achieving HIPAA compliance and protecting patient privacy and security.
FAQ’s
Is there an official HIPAA certification?
No, the U.S. Department of Health and Human Services (HHS) does not endorse an official HIPAA certification program. Compliance is self-attested, and organizations may undergo audits or assessments by third-party experts to validate their compliance efforts.
What are the penalties for HIPAA violations?
Penalties for HIPAA violations can range from monetary fines to criminal charges, depending on the severity and nature of the violation. Fines can range from $100 to $50,000 per violation, with an annual maximum of $1.5 million for each violation category.
What are the main components of HIPAA compliance?
The main components of HIPAA compliance include implementing administrative safeguards (policies and procedures), physical safeguards (physical security measures), technical safeguards (technical security measures), and organizational requirements (training, documentation, and risk management) to protect the privacy and security of protected health information (PHI).
What happens if a business associate experiences a data breach?
If a business associate experiences a data breach, they must promptly notify the covered entity. According to HIPAA regulations, the covered entity then notifies the affected individuals, the Secretary of Health and Human Services, and possibly the media of the breach.
Does the issuance of a Notice of Proposed Rulemaking guarantee that changes will be made to the HIPAA Rules?
No, the issuance of a Notice of Proposed Rulemaking (NPRM) does not guarantee that changes will be made to the HIPAA Rules. An NPRM is a formal announcement of proposed changes, and the final rule is determined after a public comment period and review by the regulatory agency, which may result in revisions or no changes at all.
HITECH ACT AND ITS IMPACT ON MODERN HEALTHCARE
In 2009, the Health Information Technology for Economic and Clinical Health or HITECH Act was signed to transform the American healthcare industry. The laws worked as a forward-thinking process of changing patient services. In this regard, the Patient Protection and...
BEST PRACTICES FOR DATA PROTECTION IN THE HEALTHCARE INDUSTRIES
In the healthcare sector, safeguarding sensitive information about patients is extremely important. Patient data includes personal details, medical histories, and treatment plans. Therefore, it must be protected and should be confidential. Thus, breaches not only...
HIPAA CONSULTANTS: WE KNOW HOW TO SECURE YOUR INFORMATION
Navigating HIPAA compliance can be complex; therefore, organizations seek advice from HIPAA consultants. These HIPAA experts have specific knowledge. They can help firms to understand the problematic standards of the Healthcare Privacy Act. In 1996, HIPAA was created....