In an age where sensitive health information is increasingly stored and transmitted electronically, safeguarding patient privacy and data security has become a paramount concern. The Health Insurance Portability and Accountability Act (HIPAA), enacted in 1996, serves as a pivotal piece of legislation in the United States, establishing guidelines and safeguards to ensure the confidentiality, integrity, and availability of individuals’ health data. PHI HIPAA must adhere to stringent rules and specifications for safely storing, transmitting, and discarding patient data.
The core essence of HIPAA revolves around the notion of Protected Health Information (PHI), encompassing vital health-related data and serving as a pivotal element in safeguarding patient privacy, fortifying data security, and fostering mutual respect between patients and medical practitioners.
This article explores the nuances of PHI under HIPAA, including its relevance, definition, legal ramifications, and necessary protections to maintain its privacy.
WHAT IS HIPAA AND ITS BENEFITS?
HIPAA stands for the Health Insurance Portability and Accountability Act, a landmark piece of legislation enacted in the United States in 1996. It was designed to improve the portability and continuity of health insurance coverage for individuals while also establishing critical safeguards to protect the privacy and security of individuals’ health information.
Benefits of HIPAA:
1. Privacy Protection: It creates federal guidelines to safeguard patients’ medical records and other PHI. It ensures that patients have control over their health information and gives them the right to access and review their medical records.
2. Data Security:It sets forth requirements for covered entities to implement administrative, physical, and technical safeguards to protect PHIHIPAA. These safeguards aim to ensure the confidentiality, integrity, and availability of ePHI, reducing the risk of data breaches and unauthorized access.
3. Healthcare Continuity: HIPAA’s provisions for health insurance portability help individuals maintain continuous health insurance coverage even during job changes or life events, ensuring uninterrupted access to healthcare services.
4. Accountability and Compliance: It requires covered entities, such as healthcare providers, health plans, and healthcare clearinghouses, to comply with the privacy and security standards. Non-compliance can lead to severe penalties, promoting accountability in handling PHI.
5. Standardization and Interoperability: HIPAA’s regulations promote the standardization of electronic health information, allowing for better interoperability among different healthcare systems, which, in turn, improves care coordination and data exchange.
WHAT IS PHI UNDER HIPAA AND ITS BENEFITS?
PHI stands for Protected Health Information. It refers to individually identifiable health information related to an individual’s past, present, or future health condition, the provision of healthcare services, or the payment for healthcare services. It can include a wide range of health data, such as medical records, test results, treatment plans, and insurance information.
The protection of PHI under HIPAA is of utmost importance in the healthcare industry to ensure patient privacy and comply with regulations The healthcare sector handles sensitive patient data, including their birthdate, medical history, and insurance claims.
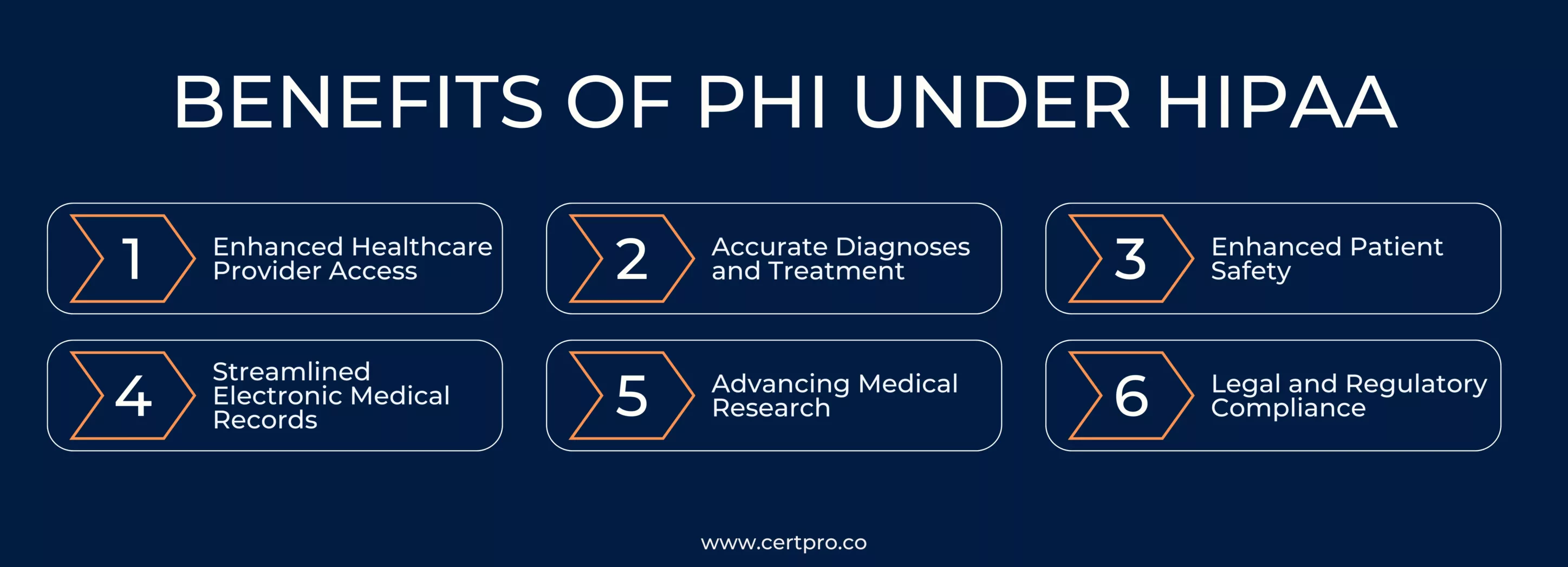
It offers several benefits in the context of PHI under HIPAA:
1. Enhanced Healthcare Provider Access: It allows healthcare providers to access comprehensive patient information, including medical history, test results, and treatment plans. This enables seamless and coordinated care across different healthcare settings, leading to improved patient outcomes.
2. Accurate Diagnoses and Treatment: Having access to complete PHI aids healthcare professionals in making accurate diagnoses and developing personalized treatment plans, resulting in more effective and efficient healthcare interventions.
3. Enhanced Patient Safety: It assists in reducing medical errors by providing healthcare providers with critical information about a patient’s allergies, medications, and medical conditions, ensuring safer and more informed decision-making.
4. Streamlined Electronic Medical Records: Electronic medical records containing PHI streamline administrative processes such as billing, scheduling, and insurance claim processing, leading to improved healthcare efficiency and reduced paperwork.
5. Advancing Medical Research: It is valuable for medical research and population health studies. It allows researchers to analyze trends, identify health patterns, and develop targeted interventions to improve public health outcomes.
5. Legal and Regulatory Compliance: Proper handling and protection of Protected health information ensure compliance with data privacy laws and regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), preventing legal penalties and reputational damage.
HIPAA PRIVACY RULE UNDER PHI
The HIPAA Privacy Rule is an essential component of the law that governs the use and disclosure of PHI. It establishes national standards for protecting the privacy and confidentiality of individuals’ health information while allowing for the appropriate flow of health information for patient care and other necessary purposes.
Key aspects of the PHI HIPAA Privacy Rule include:
1. Covered Entities: PHI HIPAA applies to covered entities, which include healthcare providers, health plans, and healthcare clearinghouses that electronically transmit Protected Health Information. It also extends to their business associates, who handle this on their behalf.
2. Patient Rights: The Privacy Rule grants patients several rights regarding their PHI. These rights include the right to access, inspect, and obtain copies of their health information, as well as the right to request corrections to any inaccuracies in their records.
3. Notice of Privacy Practices: Covered entities are required to provide patients with a Notice of Privacy Practices (NPP) that explains their privacy rights, how their health information will be used and disclosed, and the covered entity’s legal obligations concerning Protected health information.
4. Use and Disclosure: The PHI HIPAA Privacy Rule sets out specific circumstances in which covered entities can use and disclose PHI without patient authorization. These permissible uses and disclosures include treatment, payment, healthcare operations, public health activities, and certain other exceptions.
5. Minimum Necessary Rule: Covered entities must limit their use, disclosure, and requests for Protected health information to the minimum necessary to accomplish the intended purpose. This helps to protect patient privacy and reduce the risk of unnecessary exposure to health information.
6. Business Associate Agreements: Covered entities must have written agreements with their business associates outlining the responsibilities of each party regarding the protection of Protected health information.
WHAT ARE HIPAA PHI VIOLATIONS?
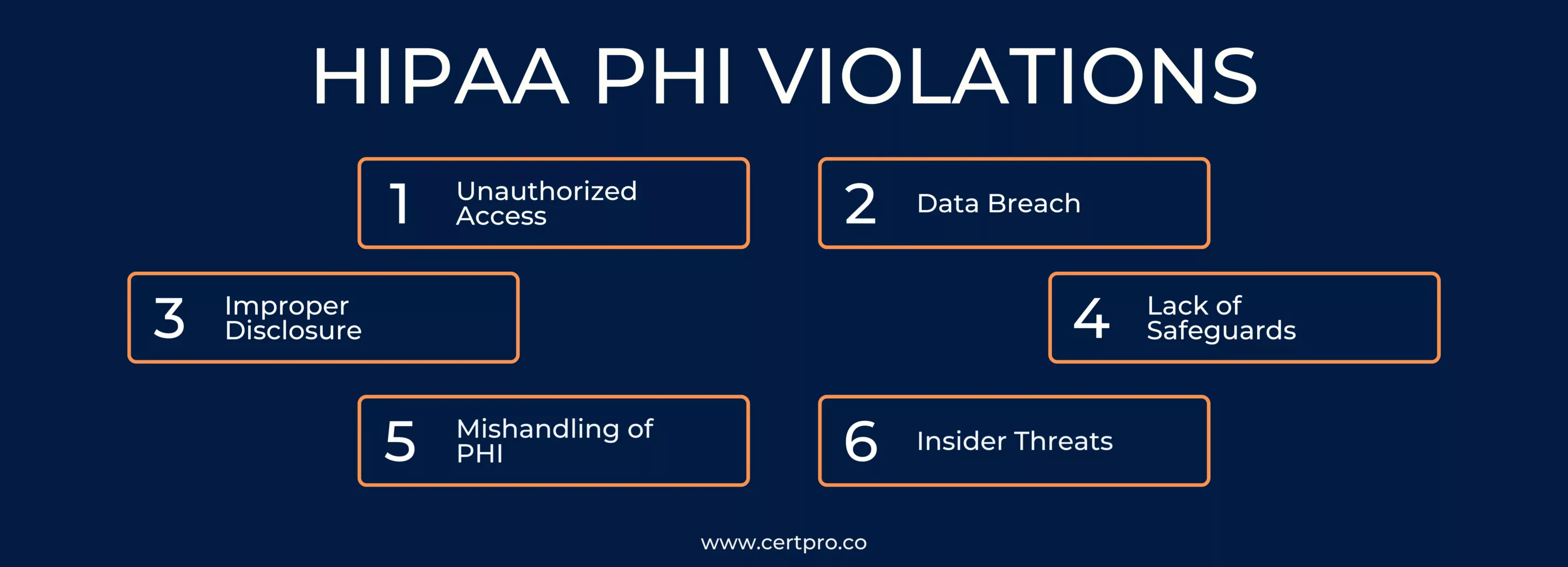
A PHI HIPAA violation occurs when there is unauthorized access, use, or disclosure of an individual’s protected health information in violation of the HIPAA regulations. It is sensitive and confidential health information, and its protection is essential to maintaining patient privacy and data security.
Examples of PHI HIPAA violations include:
1. Unauthorized Access: When an individual, such as a healthcare employee or an unauthorized person, accesses Protected health information without a valid reason or proper authorization.
2. Data Breach: If there is a security breach or hacking incident that results in the unauthorized disclosure of Protected Health information.
3. Improper Disclosure: Sharing health information with individuals or entities that do not have a valid reason or permission to access the information.
4. Lack of Safeguards: Failure to implement appropriate administrative, physical, and technical safeguards to protect health information from unauthorized access or disclosure.
5. Mishandling of PHI: Improper disposal of paper or electronic records containing health information, leading to the risk of data exposure.
6. Insider Threats: When employees or workforce members misuse or share health information for personal gain or malicious intent.
The consequences of a PHI HIPAA violation can be severe and may include civil monetary penalties, corrective action plans, and reputational damage. The Office for Civil Rights (OCR) of the Department of Health and Human Services (HHS) is in charge of upholding HIPAA laws and looking into possible infractions.
SAFEGUARDS FOR PHI PROTECTION UNDER HIPAA
HIPAA (Health Insurance Portability and Accountability Act) mandates strict safeguards to protect the confidentiality, integrity, and availability of Protected Health Information held by covered entities. These safeguards fall into three categories: administrative safeguards, physical safeguards, and technical safeguards.
1. Administrative Safeguards: These safeguards focus on the policies, procedures, and practices that govern the use and protection of health information. Covered entities are required to conduct regular risk assessments to identify potential vulnerabilities in the handling of Health Information.
2. Physical Safeguards: These safeguards are designed to protect Health Information from unauthorized physical access, tampering, or theft. Covered entities must control physical access to facilities, data centers, and areas where health information is stored or processed to ensure that only authorized personnel can enter.
3. Technical Safeguards: These safeguards focus on the technology and electronic measures used to protect and control access to health information. Covered entities must implement access controls, such as unique user IDs and passwords, to ensure that only authorized individuals can access electronic protected health information.
Implementing a comprehensive security program that addresses administrative, physical, and technical safeguards is crucial to maintaining patient trust, avoiding potential legal and financial consequences, and upholding the integrity of the healthcare industry’s commitment to patient data protection.
FAQ
WHAT IS INCLUDED IN PHI?
It includes individually identifiable health information, such as medical records, test results, treatment details, and insurance information.
HOW IS PHI PROTECTED UNDER HIPAA?
HIPAA mandates strict safeguards, including administrative, physical, and technical measures, to ensure the confidentiality and security of PHI.
WHO MUST COMPLY WITH HIPAA’S PHI REGULATIONS?
Covered entities, such as healthcare providers, health plans, and healthcare clearinghouses, must comply with HIPAA’s protected health information regulations.
WHAT ARE THE CONSEQUENCES OF UNAUTHORIZED PHI DISLCOSURE?
Unauthorized health information disclosure can lead to legal penalties, reputational damage, and a loss of patient trust for non-compliant entities.
HOW CAN COVERED ENTITIES ENSURE COMPLIANCE WITH PHI REGULATIONS ?
Covered entities must implement comprehensive security measures and provide staff training to safeguard PHI and meet HIPAA requirements.

About the Author
SHREYAS SHASTHA DRUPADHA
Shreyas Shastha Drupadha, a Senior Business Consultant. Serving as an ISO 27001 Lead Auditor, Shreyas ensures the establishment of robust information security management systems. His expertise also encompasses GDPR, HIPAA, CCPA, and PIPEDA implementation.
HITECH ACT AND ITS IMPACT ON MODERN HEALTHCARE
In 2009, the Health Information Technology for Economic and Clinical Health or HITECH Act was signed to transform the American healthcare industry. The laws worked as a forward-thinking process of changing patient services. In this regard, the Patient Protection and...
BEST PRACTICES FOR DATA PROTECTION IN THE HEALTHCARE INDUSTRIES
In the healthcare sector, safeguarding sensitive information about patients is extremely important. Patient data includes personal details, medical histories, and treatment plans. Therefore, it must be protected and should be confidential. Thus, breaches not only...
HIPAA CONSULTANTS: WE KNOW HOW TO SECURE YOUR INFORMATION
Navigating HIPAA compliance can be complex; therefore, organizations seek advice from HIPAA consultants. These HIPAA experts have specific knowledge. They can help firms to understand the problematic standards of the Healthcare Privacy Act. In 1996, HIPAA was created....